A recent decision by a federal judge in Texas has disrupted efforts to reform the Medicare Advantage program, which has come under scrutiny for significant overpayments and fraud. The ruling invalidated a regulation from the Biden administration that permitted the Centers for Medicare and Medicaid Services (CMS) to conduct more thorough audits of Medicare Advantage plans and the insurance companies managing them. This decision reflects the ongoing challenges in addressing the complexities of American health insurance, where companies like Humana have successfully contested regulations aimed at enhancing accountability.
Medicare Advantage (MA) is intended to serve as a competitive alternative to traditional Medicare, operated by private insurers who offer customized plans. However, the system is plagued by issues stemming from misaligned incentives, leading to excessive overpayments that do not benefit patients. The federal government has been footing the bill for these overpayments, with estimates indicating that insurers improperly billed the government over $19 billion in 2024 alone. This figure is expected to increase in 2025, highlighting the urgent need for reform.
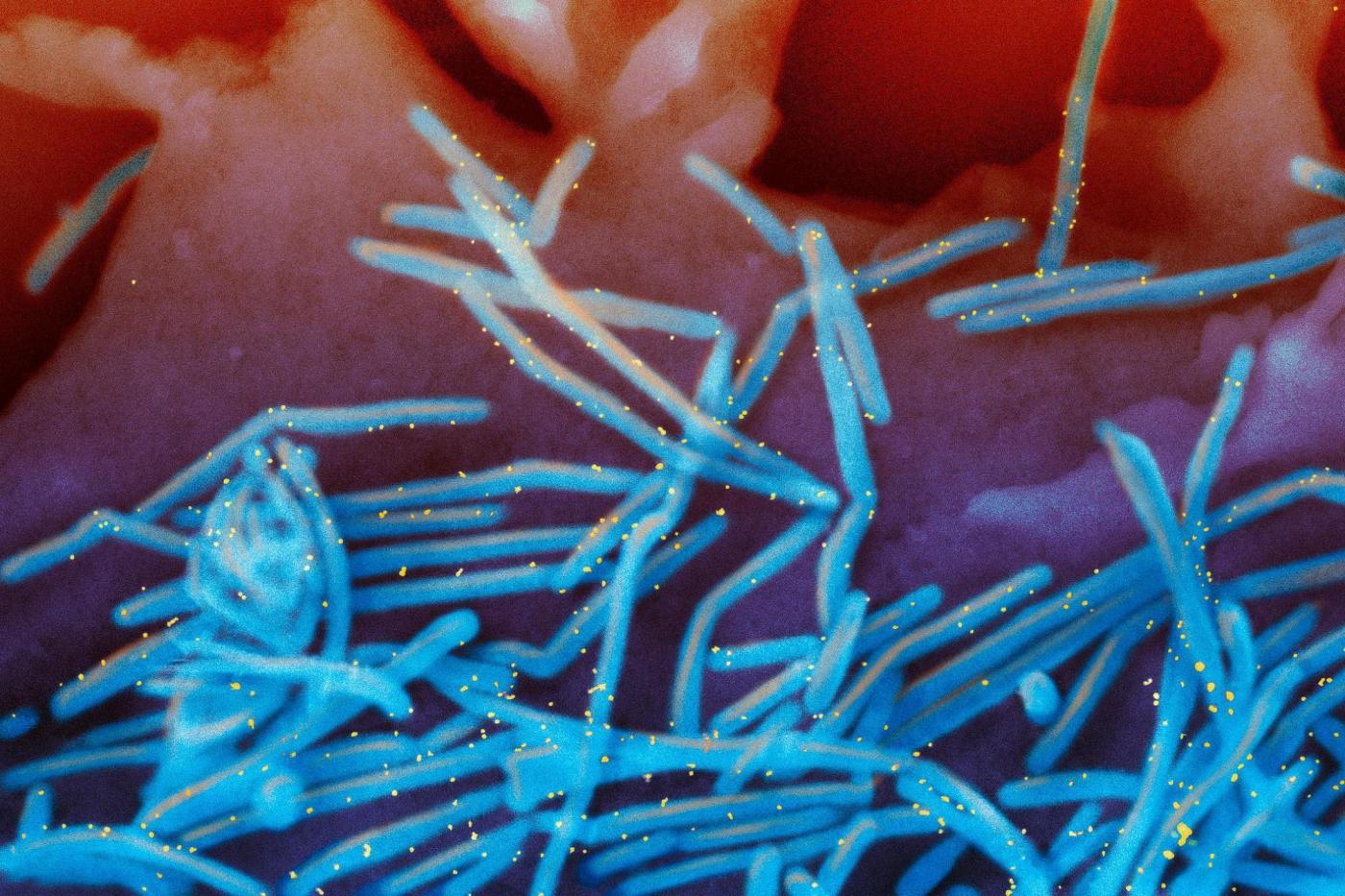
One of the primary concerns surrounding Medicare Advantage is the practice of “upcoding.” This occurs when insurers like UnitedHealthcare classify patients with more severe conditions than they actually have, inflating billing amounts. For example, a routine visit for a cold may be inaccurately billed as a serious pneumonia case. Such practices not only exploit the system but also divert funds from necessary medical care.
Another significant issue involves the risk-adjustment protocols used by insurers to categorize patients for billing purposes. Often, these assessments are conducted by non-medical personnel, raising questions about their accuracy and reliability. Insurers frequently conduct “health risk assessments,” where patients fill out questionnaires that inform their risk categorization. This process can lead to inflated claims and a focus on billing rather than genuine patient care.
According to an Inspector General’s report, approximately $7.5 billion of the improper payments in 2024 stemmed from these health risk assessments. As enrollment in Medicare Advantage is projected to surge in the coming years—potentially surpassing traditional Medicare by 2034—addressing these overbilling issues becomes increasingly urgent. Each new enrollee represents a risk for further exploitation of the system, necessitating prompt action from regulators and lawmakers.
While the recent ruling complicates oversight efforts, it does not absolve the government of its responsibility to reform Medicare Advantage. Current legislative proposals, such as the NO UPCODE Act introduced by Senator Bill Cassidy, aim to enhance the risk-adjustment model. The proposed changes would extend the duration for risk adjustments from one year to two years and limit the use of outdated conditions for upcoding. However, this bill has yet to advance beyond committee discussions, underscoring the challenges in achieving meaningful reform.
Congress now faces the critical task of enacting legislation that balances the interests of insurers with the need to protect taxpayer dollars. A collaborative approach can lead to a system that maintains the benefits of Medicare Advantage while ensuring accountability and transparency.
Dr. Juliette Madrigal, a practicing physician with 19 years of experience, emphasizes that Medicare Advantage has the potential to address many issues within American healthcare. By keeping costs in check and allowing patients to choose their preferred providers, it can serve as a viable solution. Nevertheless, to realize this potential, the program must return to its foundational free-market principles, ensuring that patient care remains the priority rather than corporate profits.