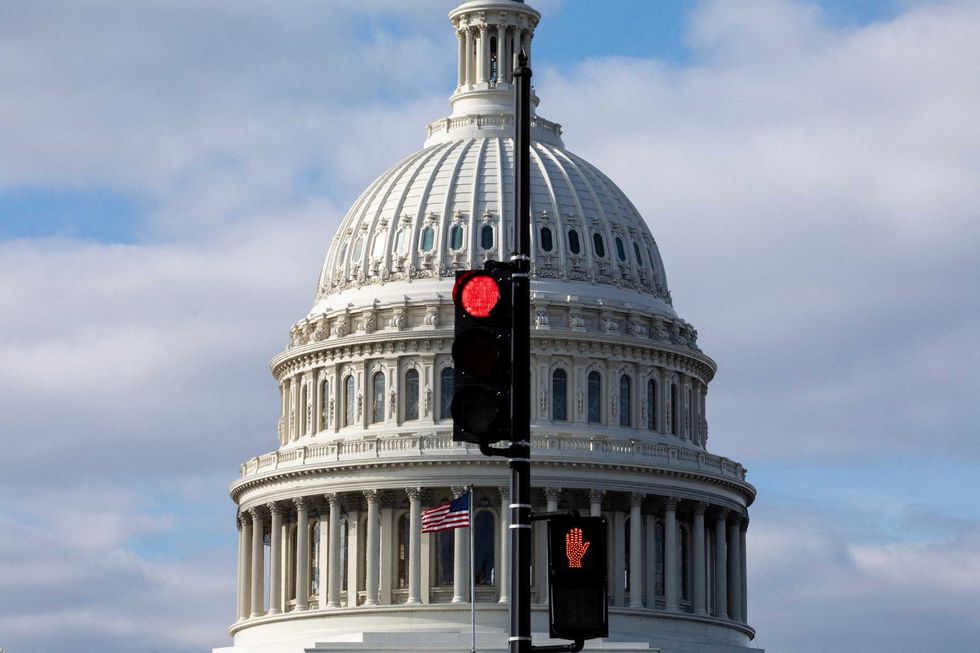
The deadline for enrolling in a marketplace plan through the Affordable Care Act (ACA) for 2026 has passed, leaving millions of Americans facing significant health care cost increases. As of December 15, 2025, no agreement has been reached regarding federal subsidies that have helped many maintain affordable health insurance. With Congress set to adjourn for the year on December 19, the situation appears dire for those reliant on these subsidies.
Disagreements surrounding health care in the United States have persisted for decades. The core issue remains whether the government, individuals, or employers should be primarily responsible for providing health care. The ACA, enacted in 2010, marked a significant shift in this ongoing debate, aiming to reduce the number of uninsured Americans, which, before its introduction, stood at approximately 49 million, or 15 percent of the population.
Impact of the Affordable Care Act
The ACA was designed to cut the uninsured rate by about 30 million, targeting a reduction to approximately 3 percent of the U.S. population. As of now, around 26 million Americans remain uninsured, representing about 8 percent of the population. This figure fluctuates according to economic conditions and changes in federal and state policies.
Two key strategies of the ACA contributed significantly to reducing the uninsured rate. The first involved expanding the Medicaid program to include individuals earning less than 138 percent of the federal poverty line. The second provided subsidies to low- and moderate-income individuals to help them purchase health insurance through ACA marketplaces.
Despite its intentions, Medicaid expansion faced considerable controversy. Initially mandated for all states, a Supreme Court ruling allowed states to opt out, resulting in only 40 states and the District of Columbia implementing the expansion, covering around 20 million individuals.
Subsidy Changes and Future Implications
The subsidies that have aided millions in acquiring health coverage are set to revert to lower levels at the end of 2025. If the enhanced COVID-19-era subsidies are eliminated, individuals earning $45,000 annually could see their health insurance payments increase by 74 percent, amounting to an additional $153 per month. Insurance plan prices are also projected to rise by approximately 18 percent in 2026, potentially leading to total increases exceeding 100 percent for many users of the ACA marketplace.
Proponents of maintaining the enhanced subsidies warn that the rollback could drive an estimated 6 million to 7 million people out of the ACA marketplace, with around 5 million becoming uninsured. This situation is exacerbated by recent policies included in a tax and spending package signed into law by former President Donald Trump in July 2025, which may lead to over 7 million individuals losing their Medicaid coverage.
The debate surrounding these subsidies has intensified, as they have significantly increased federal spending on health care. Between 2021 and 2025, the number of individuals receiving subsidies doubled, with nearly 22 million Americans benefiting from federal assistance in 2025—a 137 percent increase since 2020. Critics argue that these subsidies disproportionately aid higher earners who may not require government support.
As the nation grapples with these challenges, the need for a comprehensive health care policy remains critical. Federal and state policies continue to shape health insurance coverage, highlighting a stark contrast between states governed by different political parties. For instance, the uninsured rate among those under age 65 varies from 3 percent in Massachusetts to 18.6 percent in Texas.
Without a clear resolution to the fundamental question of who should bear the costs of health care, the United States is likely to remain entrenched in this contentious debate for years to come. The future of health care access and affordability for millions of Americans hangs in the balance as lawmakers confront these pressing issues.