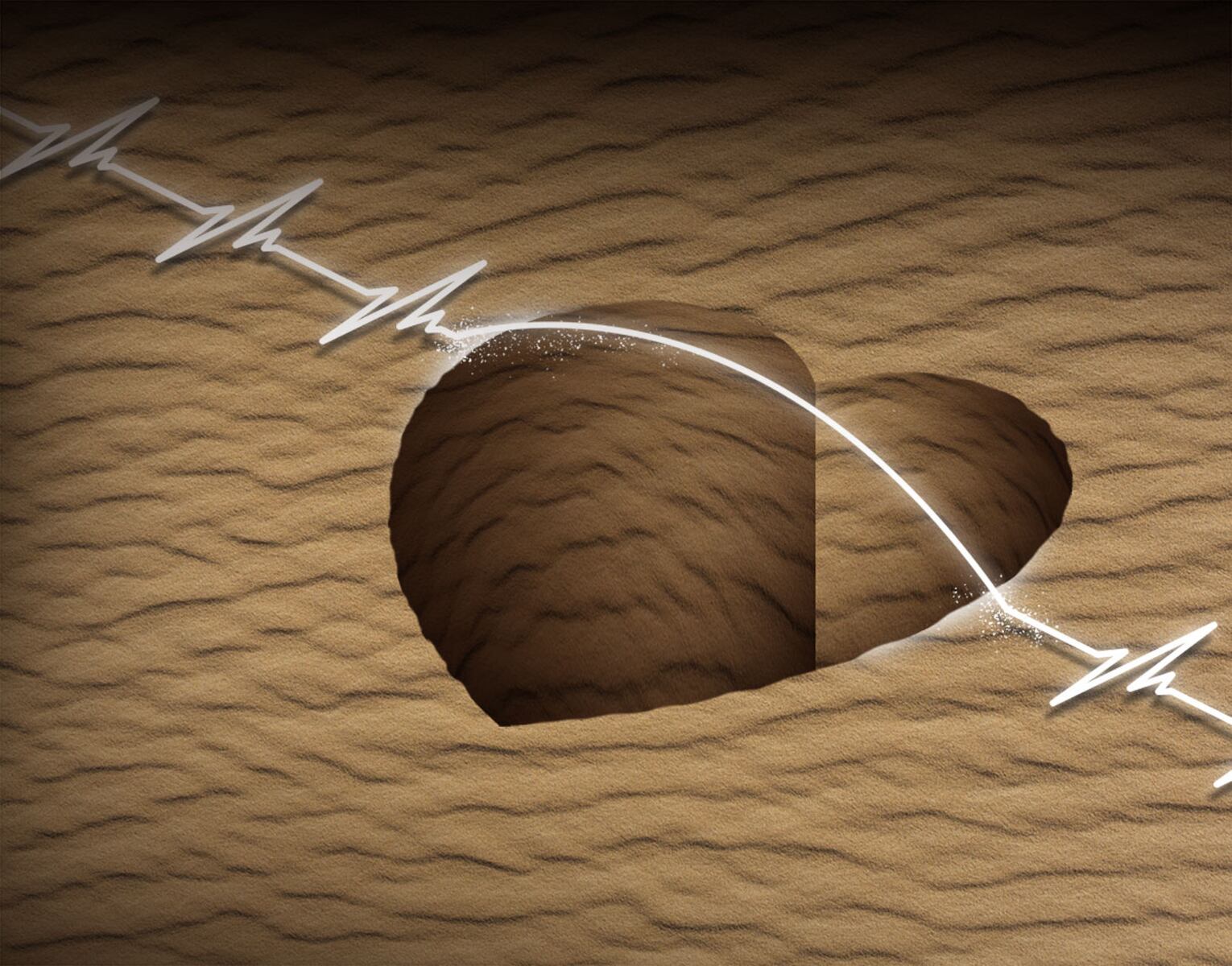
Cardiovascular disease remains the leading cause of death across various communities, with significant disparities impacting low-income individuals, women, racial minorities, and rural residents. In a recent discussion, Dr. Lee Kirksey, a Cleveland vascular surgeon and health equity advocate, emphasized the urgent need to address the so-called “cardiovascular deserts” in healthcare. These areas, characterized by a lack of access to cardiologists, primary care physicians, and specialized medical facilities, contribute to a higher prevalence of heart attacks, strokes, and other cardiovascular issues.
The term “cardiovascular desert” refers to geographic regions where healthcare resources are scarce. This scarcity often coincides with systemic barriers such as low health insurance rates and socioeconomic challenges. Individuals living in these areas face significant obstacles, including long travel times to access necessary medical care. As Dr. Kirksey notes, being physically close to advanced medical centers can be misleading; travel barriers can lead to missed work and financial strain.
Disparities in health outcomes between rural and urban communities have been widening since the 1990s, driven in part by economic decline in regions like Ohio. The exodus of manufacturing jobs during this period, particularly in the steel and automobile sectors, has left many rural areas struggling economically. Dr. Kirksey pointed out that the “rural death gap” is not just a result of geographical distance but also reflects deep-rooted economic issues.
Recent federal policies, particularly the One Big Beautiful Bill Act (OBBBA), signed into law on July 4, 2025, have raised concerns about their impact on vulnerable populations. The legislation cuts federal Medicaid spending by over $900 billion over the next decade. This reduction is expected to lead to the loss of coverage for more than 11 million individuals, according to projections from the American Medical Association. Such changes could exacerbate the already critical shortage of healthcare providers in rural areas.
In addition to funding cuts, the OBBBA has eliminated the Grad Plus Loan program, which previously enabled medical students to finance their education. This shift is likely to deter applicants from lower-income backgrounds, further deepening the physician shortage in underserved regions. Research indicates that medical students from low-income and rural communities are more inclined to return to their hometowns to practice, making this loss particularly detrimental.
On the therapeutic side, new medications like Wegovy and Ozempic have emerged as significant advancements in treating obesity and diabetes, ultimately reducing cardiovascular events. However, access to these treatments is inconsistent across different insurance types, with some patients facing out-of-pocket costs that can reach $1,000 per month. This financial burden limits access to critical innovations that could significantly benefit those in cardiovascular deserts.
Telehealth presents a promising avenue to expand access to cardiovascular care. Nonetheless, numerous challenges remain, especially regarding internet access and digital literacy in underserved communities. Establishing partnerships with broadband providers is essential to create community networks that facilitate affordable internet access. Furthermore, enhancing digital literacy among patients is crucial to ensuring they can effectively utilize remote health technologies.
Long-term telehealth reimbursement policies are necessary to incentivize healthcare systems to invest in infrastructure, best practices, and consistent provider utilization. Dr. Kirksey advocates for a collective commitment to addressing these disparities through political will, collaborative partnerships, and tailored strategies.
As he reflects on his own experiences growing up in Northeast Ohio, Dr. Kirksey urges stakeholders to remember the communities that represent the heart of the state. The existence of cardiovascular deserts highlights the urgent need for comprehensive solutions that tackle the multifaceted nature of health disparities. Addressing these issues is not just a matter of healthcare access but also of equity and justice for the most vulnerable populations.