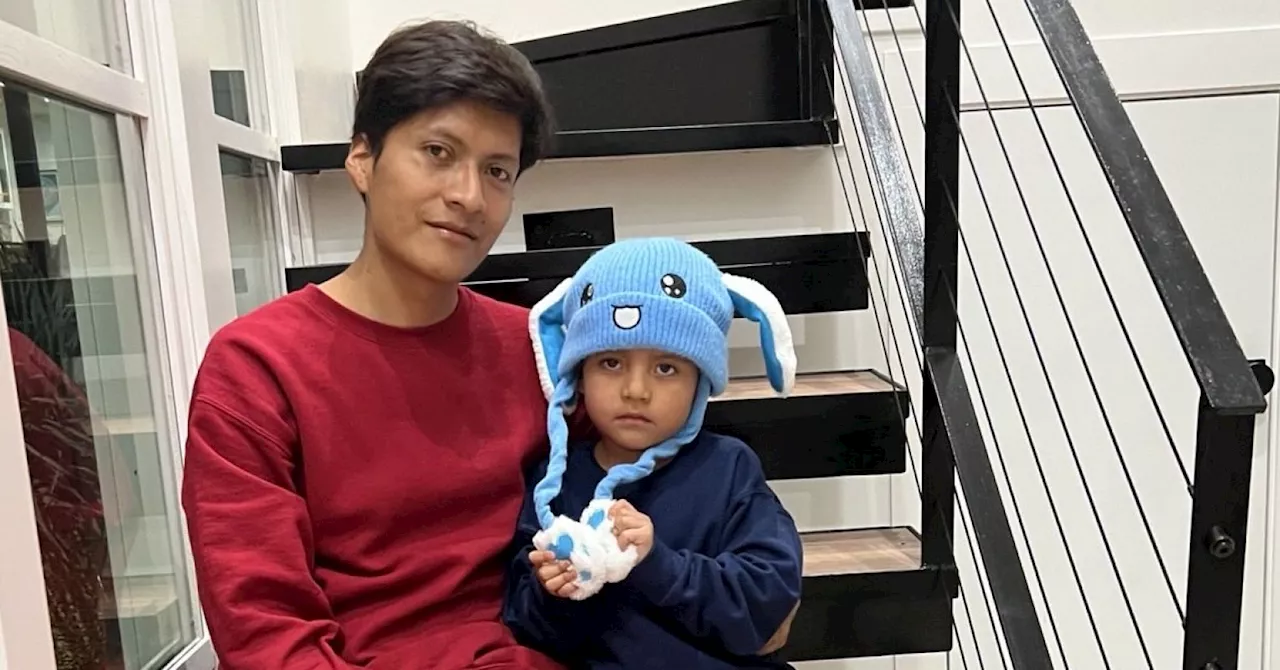
The practice of detaining children under the guise of care has come under fire as mental health providers are called to reconsider their roles in legitimizing such actions. Family separation, particularly when framed as a safety measure, can have severe long-term effects on children’s mental health, leading to conditions such as post-traumatic stress disorder (PTSD), anxiety, and depression. The recent case of five-year-old Liam Conejo Ramos, who was taken into custody by Immigration and Customs Enforcement (ICE) along with his father in January 2026, has sparked national outrage and highlighted these concerns.
On January 20, 2026, Liam and his father were apprehended in their Minneapolis suburb shortly after returning home. Their attorney claims they entered the United States legally seeking asylum but were detained unlawfully. This incident is emblematic of a broader issue: the separation of families by child welfare, juvenile justice, and immigration enforcement systems, which often occurs under the pretense of protection.
The psychological toll of such separations extends beyond individual cases, affecting entire communities. Children who witness their peers being taken away often experience profound emotional distress. For instance, one child reported threats from classmates to call immigration authorities on her family, leading to severe anxiety and ultimately contributing to her tragic death. Such experiences illustrate the pervasive fear surrounding immigration status and its impact on mental health and educational outcomes.
In their efforts to provide care, many mental health professionals inadvertently support the very systems that cause harm. These practices include mandated reporting, which can funnel families into the welfare system, and the use of diagnoses that justify criminalization. Children placed in psychiatric facilities or juvenile detention are often subjected to coercive practices that further exacerbate their trauma. Data suggest that these children, predominantly from Black and Brown communities, are more likely to receive psychiatric medications instead of the support they need.
Research within child welfare and juvenile detention settings tends to normalize family separation. Therapeutic interventions are often developed within systems that perpetuate toxic stress, leading to a cycle of harm. For example, a study found that Black parents receiving training while under surveillance reported higher levels of depression, yet recommendations focused on adding depression treatments rather than addressing the surveillance itself.
Mental health providers must grapple with their complicity in these systems. By treating detention as a site of care, they risk legitimizing the notion that healing can occur in these environments. Many providers may feel they are helping, but this perspective can obscure the reality that trauma and safety are often incompatible in detention settings.
A shift in focus is essential. Mental health professionals should advocate for alternatives to detention and prioritize keeping families together as a primary mental health intervention. This approach involves redirecting significant funding from child detention facilities to community-based supports, which can effectively reduce the risk of abuse and minimize policing.
Programs like California’s Differential Response and New York’s Family Assessment Response aim to replace investigations with voluntary support, demonstrating that family separation is not a necessity but a policy choice. Furthermore, the mental health rights and recovery movements are already developing community-based alternatives, emphasizing relationships and support outside of locked facilities.
As the situation for children like Liam Conejo Ramos unfolds, the emotional distress experienced by those in detention becomes increasingly evident. Reports of children screaming and begging to be released serve as a stark reminder of the psychological harm inflicted by family separation. Mental health providers have a crucial role to play in addressing this issue by withdrawing their support from harmful systems and advocating for community-based solutions that prioritize family unity.
The imperative to confront the systemic harms of family separation is not merely a clinical consideration but an ethical one. Healing cannot occur in confinement, and the mental health community must prioritize the well-being of children and families by redirecting efforts towards support systems that keep them together.